Hardly a day goes by without some new revelation of an information technology mess in the United States that seems like an endless round of the old radio show joke contest, “Can You Top This” except that increasingly the joke is on us. From nuclear weapons updated with floppy disks to needless deaths from medical errors, many of which are caused by preventable interoperability communication errors.
According to a report released to Congress, the Government Accountability Office (GAO) has found that the US government last year spent 75 percent of its 80 billion dollar technology budget just maintaining aging computers where floppy disks are still used, including one system for US nuclear forces that is more than 50 years old. In a previous report, the GAO outlines the challenges facing health IT interoperability.
Lack of “EHR interoperability” is not an academic issue, it impacts the healthcare of millions of Americans, and it is a major factor behind the deaths of hundreds of thousands of patients every year as a result of “medical errors.” A study from the British Medical Journal cites medical errors as the third leading cause of death in the US, after heart disease and cancer.
The GAO report, titled “EHRs: Nonfederal Efforts to Help Achieve Health Information Interoperability” details the status of efforts to develop infrastructure that could lead to nationwide interoperability of health information. The report, which was requested by Congressional leaders, describes a variety of efforts being undertaken to facilitate interoperability. The report concludes that most of these efforts remain “works in progress.” The GAO identifies five barriers to interoperability:
- Insufficiencies in health data standards
- Variation in state privacy rules
- Difficulty in accurately matching all the right records to the right patient
- The costs involved in achieving the goals
- The need for governance and trust among entities to facilitate sharing health information
CMS Pushing for ‘Plug and Play’ Interoperability Tools That Already Exist
Meanwhile in an interview with the Massachusetts Medical Society, Andrew Slavitt, Acting Administrator of the Centers for Medicare & Medicaid Services' (CMS) acknowledges in the CMS interoperability effort “we are not sending a man to the moon.”
“We are actually expecting (healthcare) technology to do the things that it already does for us every day. So there must be other reasons why technology and information aren’t flowing in ways that match patient care,” Slavitt stated. “Partly, I believe some of the reasons are actually due to bad business practices. But, I think some of the technology will improve through the better use of standards and compliance. And I think we’ll make significant progress through the implementation of API’s in the next version of (Electronic Health Records) EHR’s which will spur innovation by allowing for plug and play capability. The private sector has to essentially change or evolve their business practices so that they don’t subvert this intent. If you are a customer of a piece of technology that doesn't do what you want, it's time to raise your voice.”
He claims that CMS has "very few higher priorities" other than interoperability. It is also interesting that two different government entities point their fingers at interoperability yet ‘plug and play’ API solutions have been available through middleware integration for years, the same ones that are successfully used in the retail, banking and hospitality industries. As a sign of growing healthcare middleware popularity, Black Book Research, recently named the top ten middleware providers as Zoeticx, HealthMark, Arcadia Healthcare Solutions, Extension Healthcare, Solace Systems, Oracle, Catavolt, Microsoft, SAP and Kidozen.
Medical Errors Third Leading Cause of Death in US
The British Medical Journal recently reported that medical error is the third leading cause of death in the United States, after heart disease and cancer. As such, medical errors should be a top priority for research and resources, say authors Martin Makary, MD, MPH, professor of surgery, and research fellow Michael Daniel, from Johns Hopkins University School of Medicine. However, accurate, transparent information about errors is not captured on death certificates which are the documents the Center for Disease Control and Prevention (CDC) uses for ranking causes of death and setting health priorities. Death certificates depend on International Classification of Diseases (ICD) codes for cause of death, but causes such as human and EHR errors are not recorded on them.
According to the World Health Organization (WHO), 117 countries code their mortality statistics using the ICD system. The authors call for better reporting to help capture the scale of the problem and create strategies for reducing it. “According to the World Health’s reported by the CDC form our country’s research funding and public health priorities,” says Makary in a press release. “Right now, cancer and heart disease get a ton of attention, but since medical errors don’t appear on the list, the problem doesn’t get the funding and attention it deserves. It “boils down to people dying from the care that they receive rather than the disease for which they are seeking care.”
The Root Cause of Many Patient Errors
Better coding and reporting is a no-brainer and should be required to get to the bottom of the errors so they can be identified and resolved. However, in addition to not reporting the causes of death, there are other roadblocks leading to this frighteningly sad statistic such as lack of EHR interoperability. Unfortunately, the vast majority of medical devices, from EHRs to other healthcare IT components, lack interoperability with interoperability meaning a built-in or integrated platform that can exchange information across vendors, settings, and device types.
Various systems and equipment are typically purchased from different manufacturers. Each comes with its own proprietary operating system and its own interface technologies, just like the days before the client and server ever met. Moreover, hospitals often must invest in separate systems to pull together all these disparate pieces of technology to feed data from bedside devices to EHR systems, data warehouses, and other applications that aid in clinical decision making, research and analytics. Many bedside devices, especially older ones, don’t even connect to computers and require manual reading and data entry.
Healthcare providers are sometimes forced to take mental notes on various pieces of information in order to draw conclusions. This is time consuming and error-prone. This cognitive load, especially in high stress situations, increases the risk of error such as accessing information on the wrong patient, performing the wrong action or placing the wrong order. Because information can be entered into various areas of the EHR, the possibility of duplicating or omitting information arises. Through the EHR, physicians can often be presented with a list of documentation located in different folders that can be many computer screens long and information can be missed.
The nation’s largest health systems employ thousands of people dedicated to dealing with “non-interoperability.” The abundance of proprietary protocols and interfaces that restrict healthcare data exchange takes a huge toll on productivity. In addition to EHR’s physical inability, tactics such as data blocking and hospital IT contracts that prevent data sharing by EHR vendors are also used to prevent interoperability. Healthcare overall has experienced negative productivity in this area over the past decade.
The Devil Is in the Data Distribution
There are numerous areas in hospitals that are particularly vulnerable to deadly errors, such as acute care settings requiring a complexity of care, time critical interventions, staffing and the systems that are relied upon to tie these many IT resources together. However, due to the complexities and differences between health data systems, medical professionals are constantly presented with different user interfaces that must be consciously thought about to appropriately gather data as well as capture their decisions and treatment plans.
It is equally important to look at how the data stored in these disconnected, disparate systems is used. Much of the collection of patient, process, quality and financial data in medicine looks like a large jigsaw puzzle with a number of pieces missing. Raw data and information is fragmented across numerous non-operable EHRs, both within a single hospital or clinic along with spanning geographic ranges. Connecting these pieces has focused primarily on the transfer of the information to those who request it, a manual and error prone process that is further compounded by lack of interoperability.
Dynamic Data Flow Extends Healthcare IT
Extending the power of health IT depends on understanding the idea of data flow which is critical to the management of entire populations of patients, either within a single clinic, hospital, health system or entire community. We need dynamic data flow connected through ‘smart’ interoperable middleware pipes so we can improve on the care delivered. The flow of data can be as important, or even more important, than the individual data points and connecting the patient, the data and the interpretation depends on it.
Data flows contain signals and streams which allow automation and screening to take place. When we think at healthcare information technology from the perspective of data flow, we are not dependent on understanding every possible state or internal details, but can instead focus on the overall flow of the patient through the healthcare system. This allows for the design of complex analysis, automation and understanding that is not possible with disconnected databases.
“To build a better system for solving medical errors, we need to understand the interdependent parts of the system to create a win for the patient in better care and less redundancy, a win for the healthcare professionals enhancing and optimizing their workflow and a win for the insurance companies who are already investing a great deal of resources into care management,” says Donald M. Voltz, MD, Department of Anesthesiology and Medical Director of the Main Operating Room at Aultman Hospital in Canton, OH who is an advocate and authority on middleware.
Middleware Eliminates Need for HIEs
Now those using or considering an HIE have a new concern when the interoperability provider goes bankrupt as has happened to users of Sandlot Solutions. The MCHC-Chicago Hospital Council (MCHC), which operates the Metro Chicago Health Information Exchange (HIE) had to go to court to keep Sandlot from deleting its files until after the validation of their information was completed and delivered to MCHC. Additionally, several other Sandlot customers were dramatically affected by the same problem at significant cost to all those organizations.
As a sign of growing importance of middleware technologies in the healthcare industry, leading health IT research organization Black Book Research recently released a report on “the interoperability tangle.” In the report, managing partner Doug Brown warned that, “The misalignment of requirements and protocols has hampered all the stakeholders’ interoperability efforts. This disorder is ushering in a new replacement revolution, this time for those HIEs failing to meet the expectations of their users, payers and providers alike.”
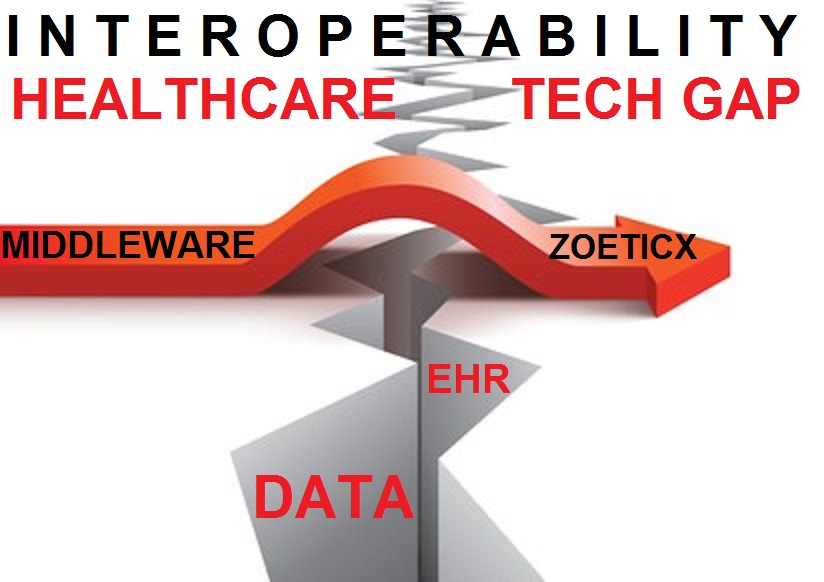
According to the announcement of the report, “In response to alleviate concerns of HIEs with poor connectivity outside their IDNs and hospital systems, interoperability middleware is also a fast growing consideration according to 16% of hospital systems IT leaders with EHR-dependent HIE grievances, in particular. Middleware is gaining popularity fast by hospitals using EHR-dependent HIE systems with extremely expensive custom development for data sharing outside the network.” Brown explained that “The middleware software sits within the data pipeline and translates data from disparate EHRs which shows promise for private HIEs, particularly payer-centric enterprise models. It creates a business intelligence layer that provides information to all stakeholders in real time.”
How to Fix This Mess
While the US technology gap will most likely continue, actions can be taken today to end the needless medical deaths. Two obvious immediate steps include:
The CDC needs to be more transparent and accountable by providing specific patient expiration details on death certificates. The ICD must also step up and add codes for human and EHR causes of death so the 117 countries using this system will have better accuracy and can help pinpoint specific problems.
As government officials continue to fail in taking a leadership role in solving interoperability, health systems operators can easily step up. Integrating EHRs with open middleware driven IT systems can begin today. By working together, vendors and healthcare administrators can end these needless deaths and concentrate of solving problems that there is no readily available solution to like cancer!



Thanh Tran, CEO, Zoeticx, Inc., a medical software company located in San Jose, CA. He is a 20 year veteran of Silicon Valley’s IT industry and has held executive positions at many leading software companies.
Edited by
Stefania Viscusi